Injuries and Navigating the Path to Healing
Traumatic Brain, Spine & Automobile Injuries
Around 70% of crash victims have mild traumatic brain injury, and the majority of them go undiagnosed.
Motor vehicle accidents are the third leading cause of Traumatic Brain Injuries (TBI) in the United States. The Centers for Disease Control recommends that anyone who receives a jolt to the head be evaluated. At Injury Treatment Centers of Kansas City, we specialize in the diagnosis and treatment of mild traumatic brain injuries caused by car accidents.
Symptoms of Traumatic Brain Injuries
- Confusion, Foggy Brain, Disorientation
- Memory disorder and amnesia
- Headache
- Sensitivity to light and sound
- Visual problems
- Poor attention / concentration
- Sleep disturbances
- Dizziness and Vertigo
- Imbalance
- Irritability, Anger, and Mood Swings
- Feelings of Depression and Anxiety
- Ringing in the ears
- Nausea and Vomiting
- Changes in Appetite
- Loss of Certain Bodily Functions
- Difficulty finding the right words when speaking

Traumatic Brain, Spine & Auto Injuries
The rehabilitation process begins with comprehensive testing and examination. These tests help us pinpoint the specific neural pathways that are not functioning properly. The description of the injury and the symptoms usually give way to the diagnosis of a mild traumatic brain injury. To diagnosis physiological problems resulting from a TBI the patient should have a very complete and comprehensive neurological examination. Then, using a variety of techniques, we strengthen those neural pathways to stimulate specific regions of the brain.
Traumatic Brain Injuries typically don’t show up on MRI or CT scans. Mild traumatic brain injuries are diagnosed with subjective complaints, questionnaires, and exam findings. At our clinic, we use the first FDA cleared EEG/ERP system to objectively confirm our TBI diagnosis. Our system is an electroencephalogram (EEG) that uses what is called an Event-Related Potential (ERP) to determine brain function. We are the only clinic in the area that uses this state-of-the-art technology.
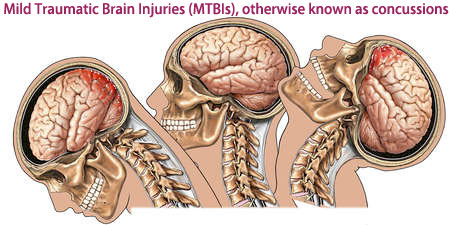
How does the brain get injured in a low-speed collision?
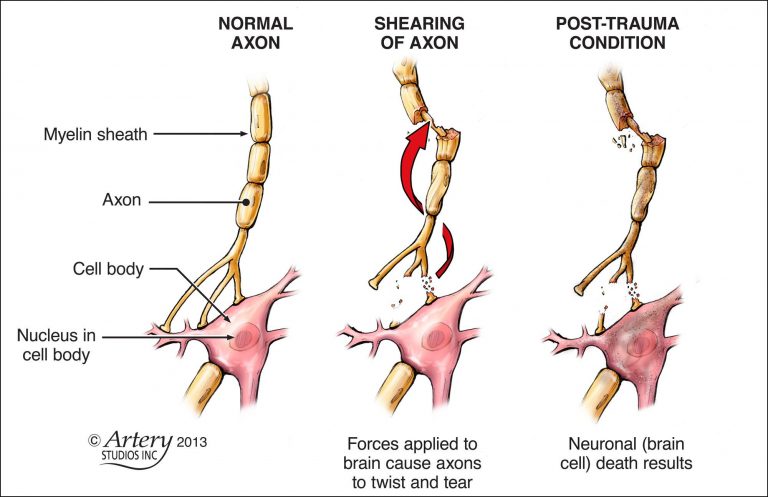
The brain is soft with the consistency of gelatin. The brain is encased inside the skull. During a crash, the movement of the skull through space (acceleration) and the rapid discontinuation of this action, causes the brain to move inside the skull. The brain moves at a different rate than the skull because it is soft. Different parts of the brain move at different speeds because of their relative lightness or heaviness. The differential movement of the skull and the brain when the head is struck results in direct brain injury due to diffuse axonal shearing, contusion and brain swelling.
Concussions
Head injuries that can cause a brief loss of consciousness and usually does not cause permanent brain injury.
Contusions
The bruising of a specific area of the brain caused by an impact to the head; also called coup or contrecoup injuries. In coup injuries, the brain is injured directly under the area of impact, while in contrecoup injuries it is injured on the side opposite the impact.
Diffuse axonal injuries (DAI)
The shearing and stretching of the nerve cells at the cellular level. It occurs when the brain quickly moves back and forth inside the skull, tearing and damaging the nerve axons. Axons connect one nerve cell to another throughout the brain, like telephone wires. Widespread axonal injury disrupts the brain’s normal transmission of information.
Although described as individual injuries, a person who has suffered a TBI is more likely to have a combination of injuries, each of which may have a different level of severity. This makes answering questions like “what part of the brain is injured?” difficult, as more than one area is usually involved. TBI case management requires very specialized and time sensitive protocols. In the absence of proper and timely treatment, serious future complications arise know as “post-concussion syndrome”.
Coup and Contrecoup Injury
Depending on the persons age, there is about .5 – 1.5″ of space between brain matter and the skull. This space is greatest in infants and toddlers. The larger space between the brain and skull, the more severe the injury. During whiplash injury, as the head and neck are thrown forward and backward, the brain is smashed against the wall of the skull. This is also known as “coup” injury.
As the head and neck whips back in the opposite direction, so does the brain. Resulting in the opposite side of the brain to also smash against the wall of the skull. This is known as a “contrecoup” injury. This injury typically happens without striking your head against any surfaces. The mere acceleration and deceleration of the head and neck cause this type of injury. Keep in mind, if the head does strike surfaces, such as an airbag, steering wheel, headrest, roof of the car, windshield, etc. the severity of injury increases exponentially.
Traumatic Brain, Spine & Auto Injuries
Victims of car collisions must be carefully evaluated for injuries to the spine and supportive tissues, which includes; bones, joints, muscles, tendons, ligaments, intervertebral discs, cartilage, and nerves.
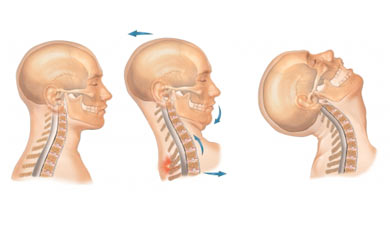
The most common ligamentous injuries to spine are caused by car accidents. Ligaments are the ultimate structures to hold vertebrae together aligned. Ligaments not only help hold the spine together, but also prevent bones from moving too far apart from each other. The kinetic energy in a car collision generates 2.5 times greater G forces to the head and neck then the bumper of the car, at a mere 8.2mph!
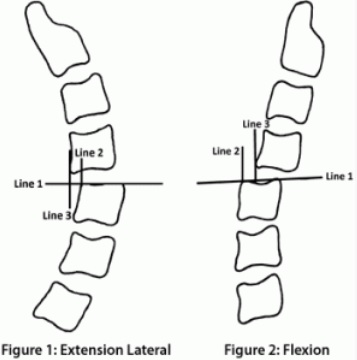
It is the shear force that causes the tearing of the ligaments, tendons, muscles, joint capsules, and nerve sheaths. This injury is also known as “whiplash”. According to AMA Guidelines, ligamentous injuries causing 3.5mm or greater slippage is awarded 25 – 28% whole body impairment.
If it’s a rear end collision, the car is jolted forward, and your body is jerked forward with it. Unfortunately, your head is not restrained so it remains at the speed it was positioned before the impact. It is the translation along the horizontal plane, which generally occurs long before the head makes contact with the head restraint, that may be the single most important factor as regards to injury potential. This high shearing force damages facet joints, discs, ligaments, and joint capsules. If a ligament is stretched beyond it’s limit, it can become torn, and in many cases it become lax because of the over stretching.
Specialized Neck X-Rays are the best way to find Ligamentous Laxity
Ligamentous laxity is one of the most concerning injuries from a car collision. Because the injury can be permanent, and it doesn’t hurt. It is imperative that ligamentous laxity is ruled out days from the accident. A missed diagnosis of this injury can be detrimental. Unfortunately, the majority of clinics treating auto accident cases are not trained to find ligamentous laxity injuries, including Emergency Rooms.
There are 4 main ligaments that are typically injured in a crash:
- Anterior Longitudinal Ligament
- Posterior longitudinal ligament
- Alar Ligament accessory atlantoaxial
- Accessory Atlantoaxial (atlantodental ligament
Think of ligaments like a plastic bag or plastic wrap. Plastic, if stretched, will not return to its normal shape again. Ligaments are the same way. Why this is so important is because when the ligament stretches too far, this becomes a permanent injury, since it will never have full strength or function the same way again.
Every whiplash injury must be graded, with grade 1 being the least severe, and grade 5 being the most severe type of injury. When there is any ligamentous injury, treatment is going take longer than a lesser grade of injury because the injury is more severe. Though every case is different, the typical treatment protocol for this type of injury is roughly 10-14 weeks of care. But depending on the amount of injury and risk factors, treatment can last many months, even up to a year.
Alteration of Motions Segment Integrity
CLICK HERE TO FIND OUT MORE INFORMATION ON AOMSI

Radiculopathy and Neuropathy
The last four spinal nerves of the neck supply the entire shoulder and arms.
The last four spinal nerves of the lower back supply the pelvis, hips, and legs.
When the neck and back are injured in a car collision, most likely one or more of these nerves sustain injuries as well. Injuries to these nerve roots cause pain, numbness, and or tingling to the arms or legs. This manifestation is known as “radiculopathy” and left untreated, becomes “neuropathy”.
Again, the treating physician is responsible to look and find these injured nerves days from the accident. This is a VERY difficult and daunting task. Because patients don’t have full blown symptoms, and to untrained eyes, undetectable to find.
ER physicians, family medical doctors, and family chiropractors do not perform in-depth mapping of the brain, spine, and spinal nerves in order to locate these hidden injuries. This is why if the patient has pain, numbness or tingling in the extremities, they must be evaluated by a physician who has trained in Neurology.
Depending on type of collision and or extent of the injuries, MRI, CT scan, and or NCV may be used to further investigate the injuries. Documentation of these neurological manifestations are also extremely important. Injuries to the brain, spine, and peripheral nerves are some of the worst injuries caused by car accidents. This is why auto insurance companies recognize these injuries as “high value drivers” in the calculation of pain and suffering settlement.

Herniated Disc Injuries and Car Accidents
Car accidents are one of the leading causes of disc injuries in the neck and lower back. It takes an injury specialist, an orthopedist, and or a neurologist to identify and diagnose herniated or bulging disc injuries.
It is important to understand that the most emergency room doctors, family doctors, and family chiropractors do not invest the time or have the expertise to identify a patient’s disc injury after an accident. Timely diagnosis and treatment of disc injuries is very important. Untreated bulging or herniated disc injuries manifest into life long pain, numbness, and tingling in the extremities, loss of muscle strength, and even more advanced neuromusculoskeletal deficits and permanent disabilities.
You must understand that it is common to have a serious disc injury and not have any aches and pains. Don’t assume that because you don’t have a lot of pain, that your discs are not herniated or bulging.
Furthermore, state and federal laws are in place to protect victims of disc injuries caused by car accidents. In addition, insurance companies take herniated and bulging disc injuries very seriously. And have assigned high cash values for pain and suffering for cases involving herniated or bulging discs caused by auto collisions.
What are bulging and herniated discs, and how are they caused by car accidents?
Simply put, spinal discs are like little pillows that are set between each vertebra in your spine. These discs are very important because they help absorb shock as you move about in your everyday life. It might help to think about spinal discs like jelly doughnuts, since they have a shell-type barrier that covers a liquid substance. Physical trauma, like the kind suffered during a car accident, can cause the disc to bulge or even rupture and let the “jelly” to bulge or even ooze out of it (herniation). At this point, it is not uncommon for the disc to shift and hit a nerve in the spinal column.
When a nerve is pinched in such a way that it causes this kind of “radicular” pain, many patients feel as if bouts of pain are shooting through the body to one specific area. Depending on the location of the bulging or herniated disc in question, this pain can be located in the leg, the arm, or other places.
However, the pain you feel as a result of disc injury may not be located in the spine—it can “radiate” to other parts of the body, depending on the particular disc that has been impacted. It is also common to have numbness running down the buttocks through the back of the thigh and into the foot when the damage is in the lower back, and into the arm, forearm, hands, and fingers when the damage is the neck.

Muscle Tearing
Nearly all auto accidents over 5 mph cause muscle tearing a.k.a. strain injuries. This happens because the head, neck, and spine get whipped around after the impact. This whipping motion causes one group of muscles to stretch on the verge of ripping out of the bone, know as the “physiological limit”, while a different muscle group will violently contract to stop the stretched muscle from tearing out of the bone. These conjugated actions always result in microscopic tearing of the muscle fibers, even at 5 mph!
These muscle injuries are most commonly found in the front and back of the neck, between the ribs, upper back, and lower back. Diagnosing and treating these muscle injuries require specific protocol well beyond medication, such as; proper immobilization, icing, slow stretch stimulation, manipulation, etc.
Comprehensive diagnosis and management of these injuries will ensure prevention of more serious neurological complications that will likely develop, such as:
- Formation of Trigger Points
- Myofascial Pain Disorder
- Loss of Strength
- Loss of Flexibility and Range of Motion